
IVF Embryo Genetic Testing
Preimplantation Genetic Testing may increase the probability of success
Preimplantation Genetic Testing (PGT) of embryos has been recommended for use alongside In Vitro Fertilization to identify and transfer only genetically normal embryos, aiming to increase the chances of a successful pregnancy.

IVF Embryo Genetic Testing
Embryo genetic testing has been suggested for patients who are at risk of an elevated probability of having genetically abnormal embryos. This includes women of advanced maternal age (35 or older).
Additionally, it may provide benefits for patients with a history of repeated early pregnancy loss (three or more), repeated failed IVF cycles despite transferring high-quality embryos (three or more transfers), and severe male factor infertility.
Preimplantation Genetic Testing (PGT) is a multifaceted treatment that involves several steps. It includes the creation of embryos through IVF, micro-biopsy of normally developing embryos, embryo cryopreservation, genetic analysis of the extracted cells (PGT), and finally, a Frozen Embryo Transfer.
The cost of adding PGT to your treatment varies depending on the type of treatment. Please contact us for pricing.

Bay IVF Services Covered in the Embryo Genetic Testing Fee

Included
- Embryo biopsy (one or more as needed)
- Preparation of cells for transport
- Cryopreservation of all biopsied embryos
Please note that the treatment fee does not cover embryo genetic analysis. You will be billed directly by an outside genetic laboratory for the analysis of the embryonic cells.
Adding PGT to IVF Duo & IVF Trio
IVF Duo and IVF Trio can provide substantial savings over the cost of regular, single-cycle In Vitro Fertilization
At Bay IVF, we understand that fertility treatments represent a significant investment toward your family’s future.
As part of our commitment to you, we are dedicated to providing pricing transparency.
Bay IVF Treatment Fees
In Vitro Fertilization (IVF)
Analgesia
Use of Procedure Room
IVF Duo

Embryo Freezing
Frozen Embryo Transfer
IVF Trio

Embryo Freezing
Frozen Embryo Transfer
Gender Selection
Embryo Freezing

Reciprocal IVF
Embryo Freezing
Egg Freezing

Second Egg Freezing

Embryo Banking IVF
Embryo Freezing
Donor Egg IVF
Embryo Freezing
Frozen Donor Egg IVF
Embryo Freezing
Gestational Surrogacy
Embryo Freezing
Frozen Embryo Transfer
Embryo Assisted Hatching
Please note that the treatment fees do not cover medications (charged by a pharmacy), pre-treatment screening evaluation, and laboratory testing required by the State of California and the FDA.
Your payment in full may be made by personal check, cash, or credit card. We are happy to provide you with physician statements for submission to your insurance company for reimbursement.
What You Do Not Have to Pay for at Bay IVF
We strive to minimize the financial impact of your fertility care. Our sole goal is to ensure the success of your treatment!
Administration of
Hormonal Injections

Some Medications for Ovarian Stimulation
Repeated Sonohysterograms

IVF Treatment Management
Repeated IVF Sperm Preparation

Use of Procedure Room for Egg Retrievals
Analgesia for Egg Retrievals
Extended Embryo Culture
Embryo Freezing

Frozen Embryo Transfer(s)

Repeated Embryo Biopsies in the same IVF cycle

Repeated Embryo Freezing in the same IVF cycle

Repeated Pregnancy Tests
IVF with PGT Treatment Process
1 — IVF to create embryos
In Vitro Fertilization procedure creates as many high-quality embryos as possible
2 — Extended embryo culture to blastocyst
By the fifth to seventh day after the egg retrieval, the embryos should reach the blastocyst stage (80 or more cells)

4 — Embryo Freezing
Since it takes several days to carry out the embryo genetic analysis, the blastocysts are cryopreserved immediately after their biopsy and stored in liquid nitrogen in our IVF laboratory

3 — Blastocyst trophectoderm biopsy
An embryo biopsy is performed by creating an opening in the eggshell around the embryo. It is possible to safely remove six to eight cells through this opening using a special microscope with micromanipulators

5 — Genetic analysis of the embryonic tissue
The genetic analysis will check for many of the most common genetic conditions and will also determine the gender of each embryo
6 —Liquid nitrogen storage of the embryos
Frozen embryos can be stored for extended periods of time, but most patients will start their Frozen Embryo Transfer cycle with the onset of the first menstrual period after their IVF treatment
7 — Subsequent Frozen Embryo Transfer
When you decide to conceive with your cryopreserved embryos, one or two genetically “healthy” embryos of the desired gender will be thawed and transferred into your uterus
Prerequisites for IVF with PGT
Only a few treatment prerequisites are needed before the start of your treatment. They assess the egg and sperm quality and ensure that embryos can be accurately placed in a healthy uterus.
Female partner’s age
The probability of a successful IVF treatment becomes exceedingly low by age 44. You must be 43 and 11 months or younger at the time your IVF treatment begins. Patients who are 44 and older should strongly consider Donor Egg IVF as the most effective treatment option to achieve a successful pregnancy.
Female partner’s weight
Your BMI must be no greater than 31 for an adequate ovarian response and safety during the egg retrieval procedure. If your BMI is higher, please follow the IVF Diet and Lifestyle (PDF) recommendations as closely as possible. By doing so, you can achieve weight loss at an optimal rate, which could significantly improve your chances of a successful pregnancy.
Pathogen testing
This testing is required by the State of California. You and your partner (if applicable) must be tested for Hepatitis B-Surface Antigen, Hepatitis C-Antibody, HIV I&II, HTLV I&II, and RPR.
Ovarian Reserve Assay (ORA)
ORA assesses the likelihood of producing normal-quality eggs. It involves measuring Follicle Stimulating Hormone (FSH), estradiol (estrogen, E2), and Anti-Mullerian Hormone (AMH) blood levels.
These test results are used to optimize ovarian stimulation.
Antral Follicle Count
The number of antral follicles (small fluid-filled sacs within the ovaries seen on ultrasound) in unstimulated ovaries is related to the quality of the eggs. Ideally, there should be approximately 20 antral follicles in both ovaries combined.
Uterine measurement and saline ultrasound
It is important to determine the length of the uterus in order to ensure the correct placement of embryos.
A saline ultrasound is utilized to rule out the presence of intrauterine polyps or fibroids.
Semen evaluation
The male partner’s semen will be evaluated at Bay IVF to determine the best laboratory method for semen preparation for egg insemination.
Parents’ genetic testing (optional)
All prospective parents should consider genetic screening for hundreds of the most common genetic diseases. Please inform us during your initial appointment at Bay IVF if you would like to have your blood sample sent for genetic screening.
IVF diet and lifestyle
Environmental factors have a significant impact on reproductive health. Please review the IVF Diet and Lifestyle document (PDF) for a comprehensive list of environmental reproductive health recommendations and a source for dietary supplements.
Single Mother Families
and LGBTQ+
We are proud to be the fertility clinic providing IVF for single mothers and LGBTQ+
FAQ — Find Answers to Your Queries
Here are some of the most commonly asked fertility-related questions. A more comprehensive FAQ selection is available on the FAQ page.
Do medications used in the IVF treatment have any side effects?
Most patients should expect minimal, if any, side effects from the medications used in In Vitro Fertilization. You should be able to continue with your everyday activities during the treatment.
How long does it take to complete a cycle of IVF?
It typically takes approximately 6 to 8 weeks from the start of your treatment to the egg retrieval and embryo transfer.
Is the egg retrieval procedure painful?
Your egg retrieval should be a very comfortable experience as we use effective pain and relaxation medications. Most patients will sleep through the 5-10 minute egg retrieval procedure. Some may experience mild menstrual-like cramping.
What is ICSI, and how does it affect my embryos?
n the Intracytoplasmic Sperm Injection (ICSI) procedure, a single sperm is directly inserted into the center of an egg. ICSI has been widely used since 1993, and approximately 2 million babies have been born worldwide without significant side effects through the use of ICSI.
I am over 40. Should I plan to do PGT?
You may consider adding Preimplantation Genetic Testing (PGT) to your In Vitro Fertilization or Donor Egg IVF treatment. If you choose to do so, it eliminates the need for amniocentesis. While adding PGT to these treatments has not been proven to improve the chances of a successful outcome consistently, it can help reduce the risk of miscarriage.
How many embryos should we transfer?
We adhere to the recommendation of the American Society for Reproductive Medicine that most patients should consider transferring only one or two embryos. While we will always provide guidance, the ultimate decision of whether to transfer one or two embryos will be up to you.
Is bed rest recommended after an embryo transfer?
From a conception standpoint, it is not recommended to rest immediately after embryo transfer. Recent studies have shown that remaining active and moving around after the transfer can increase the probability of implantation. Therefore, it is advised to start moving around immediately after your transfer.
I am from the LGBTQ+ community. Can I have my treatment at Bay IVF?
Yes! We take pride in being one of the first fertility clinics in Northern California to offer In Vitro Fertilization services for lesbian partners. Our clinic is LGBTQ+ friendly and experienced in both lesbian IVF and Reciprocal IVF.
Treatments at Bay IVF
In Vitro Fertilization
In Vitro Fertilization
We use gentle and individualized ovarian stimulation protocols prioritizing egg quality over quantity. This approach minimizes clinic visits and reduces the risk of ovarian hyperstimulation without compromising the chances of a successful outcome.
A complete IVF treatment cycle can take as little as six weeks and only requires a few brief visits to the Clinic.
The cost of In Vitro Fertilization at Bay IVF is $11,870.

Gender Selection

Gender Selection
We were one of the first fertility clinics in the San Francisco Bay Area to offer Gender Selection IVF.
IVF for Gender Selection uses a Pre-implantation Genetic Testing (PGT) procedure to determine the gender of each embryo.
Through this method, prospective parents will know the gender of each embryo with 100% accuracy before transferring them into the uterus.
The cost of adding the Gender Selection procedure to IVF treatment is $4,820 at Bay IVF.

Reciprocal IVF
Reciprocal IVF
In reciprocal lesbian IVF, one partner assumes the role of the Genetic Mother by providing the eggs retrieved during the IVF cycle, while the other partner serves as the Birth Mother who carries the pregnancy.
The eggs obtained from the Genetic Mother are fertilized with donor sperm within a laboratory setting. Subsequently, the resulting embryos are transferred to the uterus of the partner who will carry the pregnancy.
This method enables both partners to actively participate in the creation and gestation of their child, fostering a deep sense of involvement and connection.
The cost of Reciprocal IVF at Bay IVF is $14,450.

Egg Freezing
Egg Freezing
The success of the egg-freezing procedure primarily depends on the patient’s age at the time her eggs are frozen.
The treatment involves retrieving eggs from the ovaries, cryopreserving them, and storing them in liquid nitrogen.
It is important to note that the probability of a successful outcome from cryopreserved eggs remains independent of the patient’s age when the eggs are thawed, inseminated, and the resulting embryo(s) transferred into the uterus.
The cost of Egg Freezing at Bay IVF is $7,750.

Pre-Implantation Genetic Testing (PGT)
Pre-Implantation Genetic Testing (PGT)
PGT can be added to IVF, Donor Egg IVF, and Embryo Banking treatments. It aims to increase the probability of a successful outcome by minimizing the likelihood of transferring genetically abnormal embryos.
Embryo genetic testing has been recommended for patients of advanced maternal age (35 or older), those with a history of repeated early pregnancy loss (three or more), and individuals who have experienced multiple failed IVF cycles despite the transfer of high-quality embryos.
The cost of adding PGT to your treatment varies depending on the type of treatment. Please contact us for pricing.

Male Infertility
Male Infertility
Approximately 10% to 15% of men are born with some degree of male infertility, and about one-third of the time, a couple’s infertility can be solely attributed to male infertility.
In recent years, the chances of infertile men conceiving their genetic child have significantly improved. In situations where patients previously had to rely on donor sperm, we can now almost always utilize the partner’s sperm to fertilize the eggs with ICSI.
The cost of adding ICSI to IVF is $2,340 at Bay IVF.

Embryo Banking
Embryo Banking
Some couples may delay starting their family to the extent that when they finally decide to have children, it can be challenging, if not impossible, to conceive naturally. Embryo Banking can be a valuable option for postponing parenthood while pursuing educational and professional goals.
Embryo Banking involves the retrieval of eggs from the ovaries, fertilization with the partner’s semen, cryopreservation of the resulting embryos, and their storage at our Clinic for future use.
The cost of Embryo Banking at Bay IVF is $14,090.

Egg Donation
Egg Donation
Egg Donation can be a highly successful treatment used by patients who no longer have high-quality eggs. Children conceived with the help of donor eggs are genetically linked to the male partner and the egg donor, while the female partner is the one who becomes pregnant, nourishes the baby throughout the pregnancy, and experiences childbirth.
You have the option to choose an egg donor from an egg donor agency or purchase frozen donor eggs from an egg bank.
The cost of the Donor Egg IVF procedure is $14,090.
Frozen Donor Egg IVF is $11,910 at Bay IVF.

Gestational Surrogacy
Gestational Surrogacy
There are numerous reasons why individuals and couples turn to gestational surrogacy. The most common are:
– Same-sex male couples
– Men who are single parents
– Women with previous hysterectomy
– Medical conditions making being pregnant too risky
The intended parents’ eggs or donor eggs are fertilized with sperm through In Vitro Fertilization. The resulting embryo is then transferred to the surrogate, who carries the pregnancy and delivers the child.
The cost of Gestational Surrogacy is $15,570 at Bay IVF.

Frozen Embryo Transfer
Frozen Embryo Transfer
Fertility treatments may involve embryo freezing and the storage of embryos in liquid nitrogen. Later on, the stored embryos can be thawed and transferred into the uterus. The processes of embryo cryopreservation, storage, and Frozen Embryo Transfer are done on-site at Bay IVF.
Frozen Embryo Transfer is very safe. Hundreds of thousands of babies have been born worldwide from cryopreserved embryos.
The cost of Frozen Embryo Transfer at Bay IVF is $4,270.

Sperm Aspiration IVF
Sperm Aspiration IVF
Some men either do not produce sperm at all or produce them in insufficient numbers and low quality. Many of these men can have their sperm directly aspirated from their testicles or the epididymis (tightly coiled tubules attached to the top of the testes that store sperm before ejaculation).
The two most common indications for sperm aspiration are a previous vasectomy and the congenital absence of the epididymis.
The fee for Sperm Aspiration IVF varies depending on the patient’s underlying diagnosis. Please contact us for pricing.

Fertility Tests
Fertility Tests
Your reproductive history and the results of your testing will determine the most likely and cost-effective treatment for achieving pregnancy.
We plan your fertility testing based on three categories of infertility factors: (1) Male factor infertility, (2) Ovulation and egg quality disorders, and (3) Uterine and Fallopian tubes factors.
Whenever possible, we utilize fertility test results conducted prior to your becoming a patient at Bay IVF to minimize your costs.
The cost of fertility testing depends on the tests performed. Many hormonal test charges are already included in the treatment fees.

We look forward to meeting you at Bay IVF and, when your treatment is successful, celebrating your new pregnancy!
 +
+Years of Experience
 +
+Babies Born
 %
%Compassionate Care
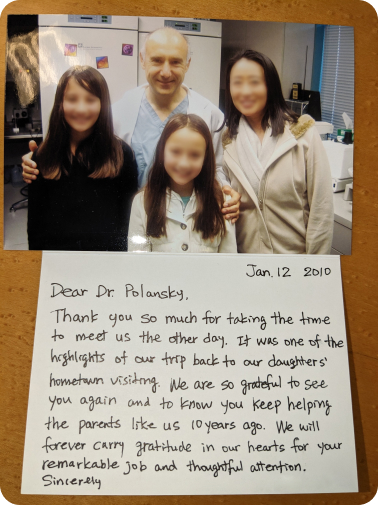
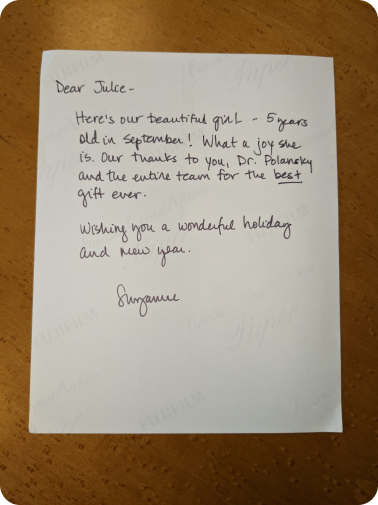
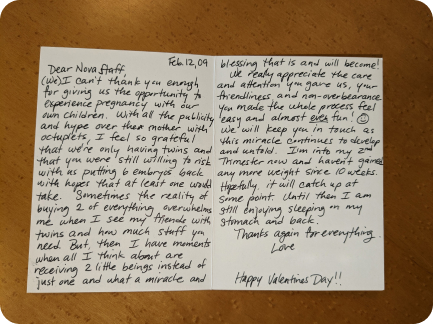
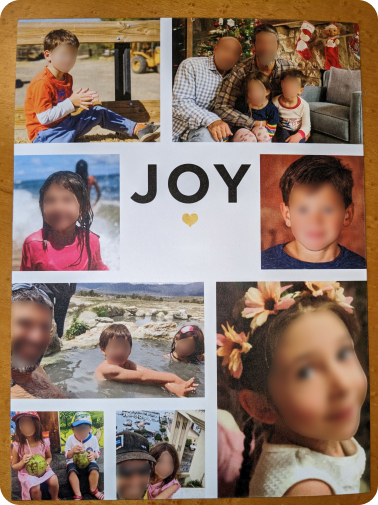
Hear from Our Patients’ Journey to Parenthood at Bay IVF!
I would highly recommend Bay IVF for those wanting to build their family and needing IVF support! Dr. Polansky and the whole Bay IVF team were so supportive and welcoming while also honest and realistic. Our girl is our dream come true!
Jennifer C.-F.This clinic has been amazing to work with. All the nurses and staff made sure I was always comfortable and were there to answer questions any time I needed. We are incredibly grateful to Dr. Polansky and the team for everything they did for us.
Harpreet K.Words could never express the gratitude my husband and I will always have for Bay IVF! We did our research and decided to check out Bay IVF. We scheduled a consultation and felt an instant connection… love at first sight!
Chelsea L.
Bay IVF Early Pregnancy Heartbeat

Meet Your Doctor

- Dr. Polansky received his medical diploma from Charles University in Prague, the Czech Republic, in 1978.
- After completing his OB/GYN residency at Jewish Hospital in Saint Louis, MO, he graduated from the Reproductive Endocrinology and Infertility (REI) fellowship at Stanford University in 1985.
- In the same year, he co-founded the Stanford IVF Clinic.
- Dr. Polansky obtained board certification in Obstetrics and Gynecology in 1986 and became REI subspecialty board certified in 1988.
- In 1987, he left Stanford University and established Nova IVF.
- In 2011, he founded Bay IVF, where he provides advanced fertility treatments with a holistic approach, utilizing state-of-the-art techniques.
- Dr. Polansky personally performs ultrasound examinations, egg retrievals, embryo transfers, and ovarian and endometrial stimulations for his patients.
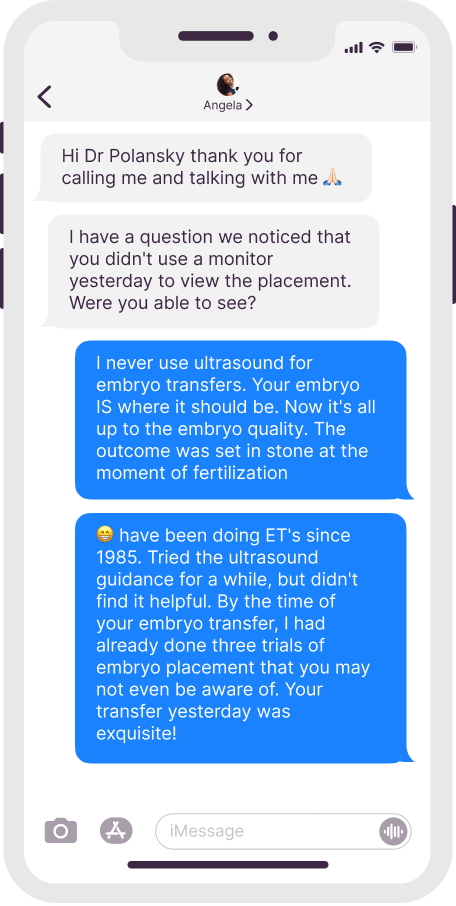
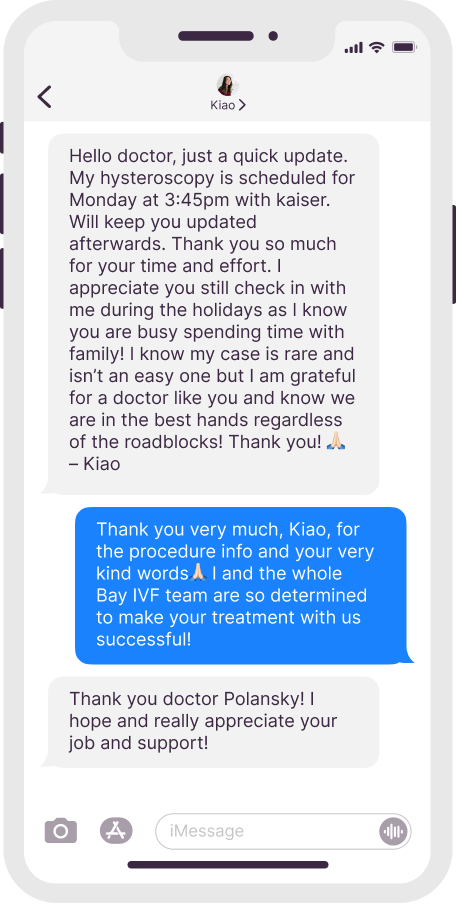
- He is deeply committed to his patients and freely shares his cell phone number, ensuring accessibility and availability 24/7.
Frank Polansky, M.D.
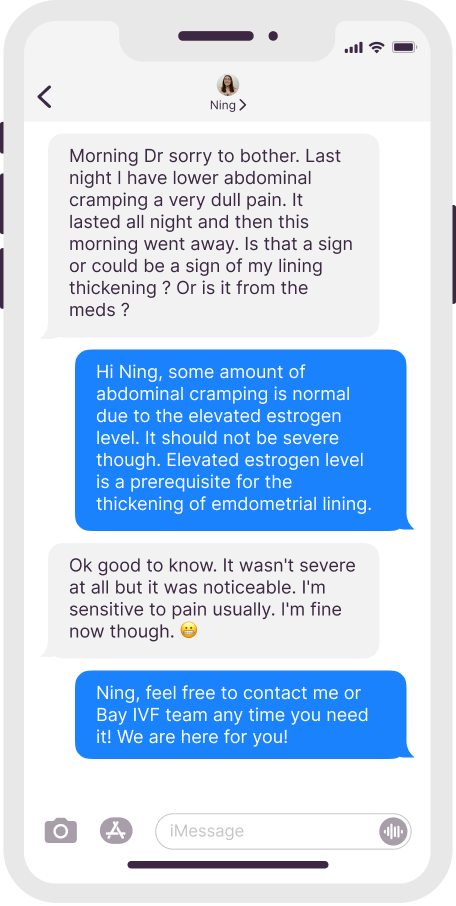
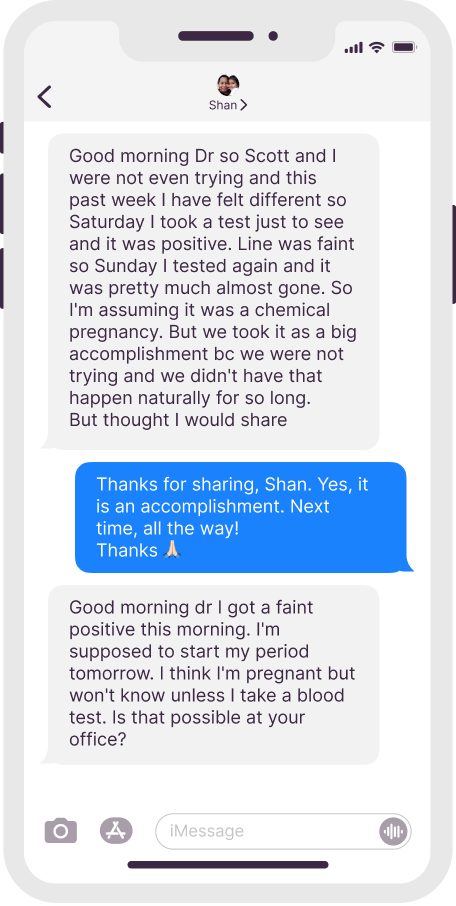
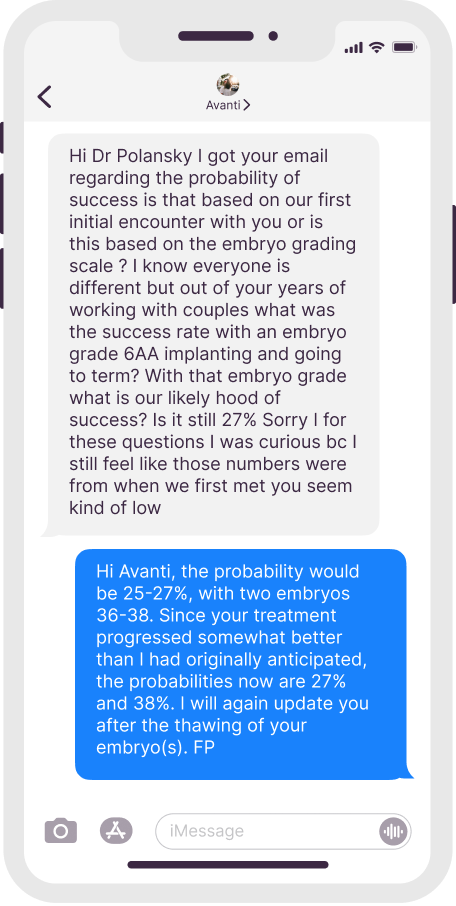
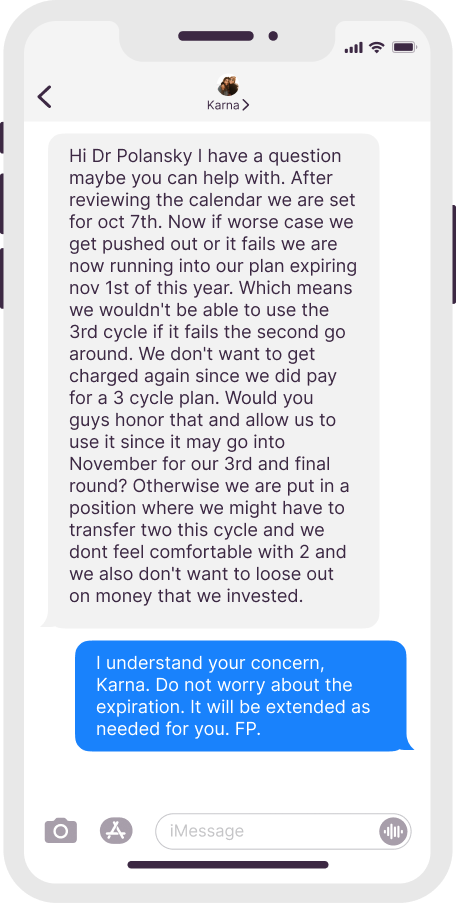
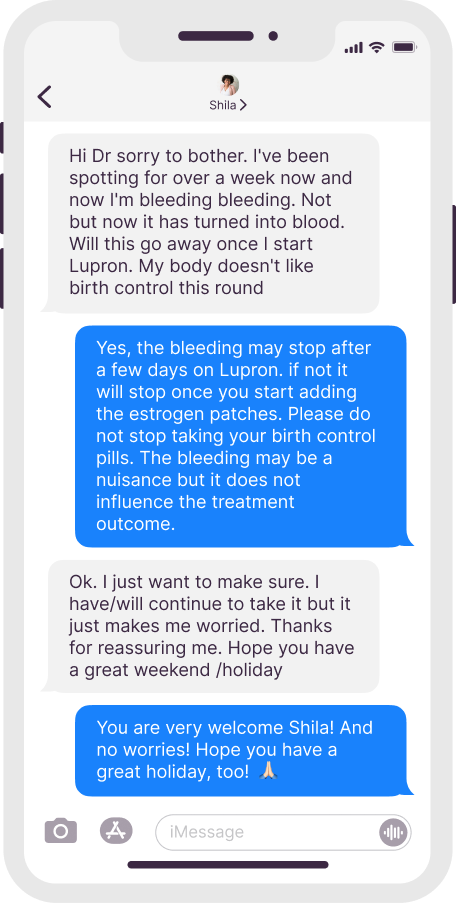
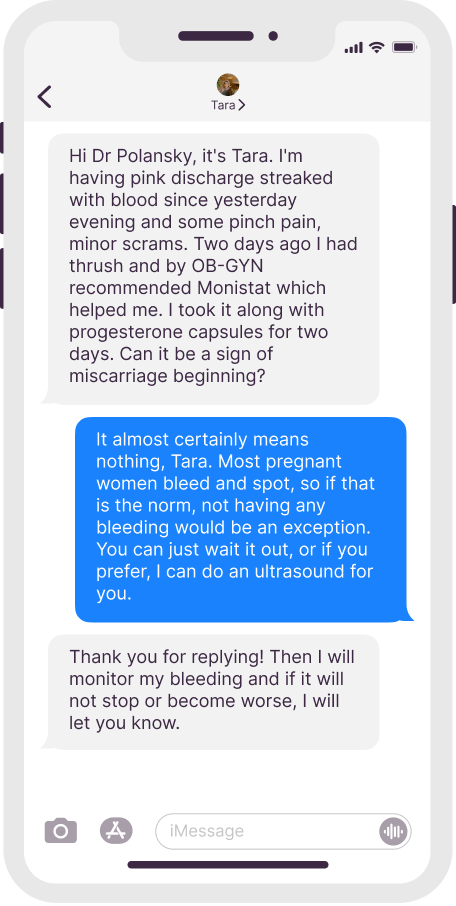
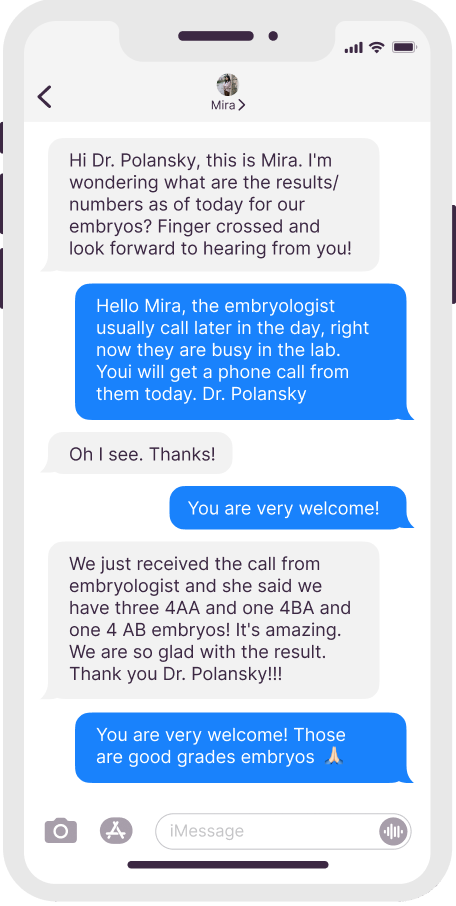
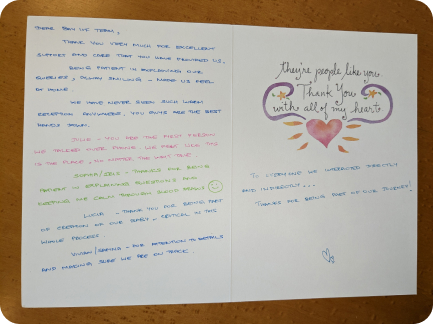
Dr. Polansky’s Communication With Patients
Real texts, anonymous patient names

Initial Appointment Questions
When you call to schedule your consultation, one of our Front Office Coordinators will ask you a short series of questions regarding your reproductive history.
Patients’ Thank You Cards


Your Initial Visit at Bay IVF
Attending a new patient appointment at a fertility clinic can be stressful. Our primary objective is to ensure that your initial visit is friendly and relaxing. We encourage you to ask questions at every step of the process.
1 — When You Arrive
You will be welcomed by one of the clinic receptionists. One of our nurses will measure your height and weight and take your blood pressure

2 — Meet Your Doctor
Dr. Polansky will ask you a series of clarifying questions and then provide you with a summary of the factors contributing to your infertility

4 — Exam Room
One of the nurses will escort you to an examination room. Your examination will begin with listening to your lungs and heart

3 — Ask Your Questions
You will then have a discussion with him about the most suitable reproductive treatment(s) for you. During this time, you will have the opportunity to ask any questions you may have

5 — Ultrasound of the Ovaries
The next step is a pelvic ultrasound to examine the uterus and ovaries. This ultrasound will help determine the number of antral follicles present within the ovaries

6 — Financial Part
Following that, you will have a discussion with one of the financial advisors regarding the financial aspects of your treatment, including potential treatment financing options

8 — Support 24/7
If you have any questions after leaving the clinic, please feel free to reach out to us via phone call, text, or email. Open and discreet communication is an integral part of the care we provide at Bay IVF

7 — What About Time?
Your entire visit is expected to last approximately one hour
Schedule Your Initial Consultation With Dr. Polansky
Online (free) or In-Person
Call or Text Us: 650-322-0500
You can also complete the form below to request your initial consultation
Still Have Questions?
We understand that this is a significant decision, and it is important to us that you feel truly comfortable









