
Frequently Asked Questions
Find Answers to Your Queries
While this FAQ section covers our patients’ most common questions, it may not answer all your queries.
If you can’t find the answer you’re looking for, don’t hesitate to contact us for assistance.
FAQ
These are the most commonly asked fertility-related questions.
Do medications used in the IVF treatment have any side effects?
Most patients should expect minimal, if any, side effects from the In Vitro Fertilization medications. You should be able to continue with your everyday activities during your treatment.
How long does it take to complete a cycle of IVF?
It takes approximately 6 to 8 weeks from the beginning of your treatment to egg retrieval and embryo transfer.
Is the egg retrieval procedure painful?
Since we use strong pain and relaxation medications, your egg retrieval should be very comfortable. Most patients will sleep through the 5-10 minute procedure. Some may experience minimal menstrual-like cramping.
What is ICSI, and how does it affect my embryos?
In the Intracytoplasmic Sperm Injection procedure, a single sperm is inserted directly into the center of an egg. ICSI has been used extensively since 1993, and approximately 2 million babies have been born worldwide without significant side effects using ICSI.
I am over 40. Should I plan to do PGT?
You may consider adding Preimplantation Genetic Testing (PGT) to your In Vitro Fertilization or Donor Egg IVF treatment. If you do, you will not need to do amniocentesis if you conceive.
Adding PGT to these treatments has not been shown to reliably improve the probability of a successful outcome, but it can reduce the probability of a miscarriage.
How many embryos should we transfer?
We follow the recommendation of the American Society for Reproductive Medicine that most patients should transfer only one or two embryos. We will always provide guidance, but you will have the final say in whether to transfer one or two embryos.
Is bed rest recommended after an embryo transfer?
It is not recommended from the conception point of view. Recent studies showed that resting after embryo transfer decreases the probability of implantation. You should start moving around immediately after your transfer.
I am from the LGBTQ+ community. Can I have my treatment at Bay IVF?
Yes! We are proud of being one of the first Northern California fertility clinics to provide In Vitro Fertilization for lesbian partners. We are a very friendly LGBTQ+ fertility clinic quite versed in lesbian In Vitro Fertilization and Reciprocal IVF.
How long should I wait before seeking treatment?
It is important that you do not wait too long before seeing an infertility specialist. Please note that there is no distinction between having unprotected intercourse and “trying” to conceive. They both represent “exposure” to conception.
35 or younger 12 months
36 – 37 9 months
38 – 39 6 months
40 – 41 3 months
42 and older Immediately
How can I increase my chance of pregnancy?
Your state of reproductive health can play an important role when trying to conceive. Please review the IVF Diet and Lifestyle (PDF) document and follow the recommendations as closely as possible.
Should I go straight to IVF or consider other treatments first?
The decision of which treatment is the most appropriate for you is based on your past reproductive history, the results of your fertility testing, and the outcome of any previous reproductive treatments you may have had. You may need In Vitro Fertilization treatment if any of the following apply to you:
History of tubal blockage and pelvic adhesions
Male Factor Infertility
Infertility associated with endometriosis
Infertility associated with Polycystic Ovary Syndrome (PCO)
Unexplained infertility
Long-standing infertility: no contraception for more than a year and a half
Decreasing “ovarian reserve”: IVF may be the most appropriate treatment for women over the age of 37.
You did not become pregnant with intrauterine insemination (IUI) cycles.
You did not become pregnant with ovarian stimulation cycles with oral or injectable medications.
Is the Sonohysterogram required?
Sonohysterogram (saline ultrasound, water ultrasound) is an essential part of treatment prerequisites. It evaluates the health of the endometrial cavity.
The endometrial cavity must be free of polyps, scarring, and myomas (fibroids) before any treatment can be initiated. Any of these structures inside the uterus could significantly compromise the likelihood of embryo implantation.
Sonohysterogram is a quick and mostly painless procedure at Bay IVF. A thin, soft catheter is passed through the cervix into the uterus, and a small amount of sterile saline solution is gently instilled. A transvaginal ultrasound is used to confirm the absence of polyps, scarring, or fibroids inside the uterus.
Until what age should I consider the IVF procedure?
The probability of a successful IVF treatment becomes exceedingly low by age 44. You must be 43 and 11 months or younger at the time your IVF treatment begins. Patients who are 44 and older should strongly consider Donor Egg IVF as the most effective treatment option to achieve a successful pregnancy.
Do I have to be legally married to have treatment at Bay IVF?
You do not. At Bay IVF, we do not discriminate based on marital and family status, gender identity, gender expression, sexual orientation, or genetic characteristics.
We have already had several IVF cycles at another clinic. Is there any hope that we will be successful with you?
Although the IVF procedure has by now become almost standardized, there are still subtle differences among IVF centers. Such slight differences may play a significant role for some patients. Therefore, we do not recommend doing more than three unsuccessful IVF cycles at any one clinic. If you have not succeeded, it is time to move on.
I am overweight; could this be a problem for the IVF procedure?
Unfortunately, yes. Increased maternal weight can have a profound negative effect on the IVF procedure and its outcome:
More medication needed to stimulate the ovaries
Lower egg quality
The safety of the egg retrieval procedure
Decreased uterine receptivity
Increased risk of baby’s heart defects
At Bay IVF, we recommend that patients adhere to our reproductive health guidelines (PDF). They can optimize health, may improve the quality of eggs and sperm, and would result in a gradual weight loss and arriving at one’s ideal BMI.
How long does it take to complete Frozen Embryo Transfer Treatment?
The Frozen Embryo Transfer (FET) procedure is much shorter than an In Vitro Fertilization cycle. It usually takes only 5-7 weeks to complete a cycle of FET, and only two clinic visits are needed.
How long can you store frozen eggs and embryos?
There is no time limit on storing cryopreserved eggs or embryos. They are stored in liquid nitrogen at close to absolute zero degrees temperature and do not age.
Your uterus does not “grow old.” Theoretically, there is no limit on the age of the recipient mother of frozen-thawed eggs or embryos.
Since pregnancy complications, not related to the uterus, increase significantly with age and could compromise the mother’s and baby’s health, you must be 48 and 11 months or younger at the time of transfer of your frozen-thawed eggs or embryos at Bay IVF.
Do I need to take breaks between treatment cycles?
Treatments that require ovarian stimulation (IVF) require a resting cycle before another cycle of treatment can begin. Whether you rest your ovaries just for one or several menstrual cycles does not make a difference. Other treatments (Donor Egg IVF, Frozen Embryo Transfer) do not require a resting cycle, and your new treatment cycle can start right away.
How many cycles of treatment should I plan for?
We typically do not recommend more than three cycles of IVF and Donor Egg IVF treatment. The number of treatment cycles you should plan for is ultimately a personal choice, but we will help you with your decision.
The lower the probability of a successful outcome per treatment cycle, the more treatment cycles you should be planning for. Most patients can increase their cumulative pregnancy probability by having more than one cycle of treatment.
Once you have completed your treatment prerequisites, we will be able to estimate your probability of success and help you with your decision.
Do you provide loans for fertility treatments?
Bay IVF has partnered with Future Family offering easy, personal, and affordable fertility care financing. Their mission is to make fertility care more accessible and affordable. Future Family loans are an alternative to high-interest credit cards and dipping into your savings.
They offer 0% APR financing for those that are eligible, as well as low monthly payment plans. Prequalifying is risk-free, easy, and will not affect your credit score.
They can help you navigate the sometimes challenging financial journey and answer all your financial loan questions. Future Family lessens your “how am I going to pay for my treatment costs” stress, which allows you to enter your treatment focusing solely on growing your family.
What kind of testing is required for Advanced Reproductive Treatments?
Semen evaluation
Ovarian reserve testing
Evaluation of the Uterus
Testing Required by the State of California and FDA
What is Ovarian Hyperstimulation Syndrome (OHSS)?
Any patient undergoing ovulation induction is at risk of developing OHSS, although some more than others. Ovarian hyperstimulation syndrome may be classified as mild, moderate, or severe by symptoms and signs.
The symptoms usually begin four to five days after the egg retrieval. A majority of women have a mild or moderate form of the syndrome, which invariably resolves within a few days. Patients may complain of abdominal discomfort and mild abdominal swelling. In a small proportion of women, the degree of discomfort can be pronounced. If a pregnancy occurs, it may delay recovery.
What happens if I have extra embryos that I do not transfer?
There may be more embryos than the future parents wish to have transferred. It is possible to cryopreserve (freeze, vitrify) these embryos and store them in liquid nitrogen. The majority of the embryos will survive the cryopreservation and thawing process. The implantation rate of the surviving embryos is similar to the “fresh” embryos.
Are there increased birth defects in IVF or Donor Egg IVF babies?
There is an extensive number of published reports documenting no correlation between children conceived with medical intervention and birth defects. These are real and natural babies; they will kick, spit-up, scream, and keep you up all night just like any other baby.
What is unexplained (idiopathic) infertility?
Up to 25% of all infertile patients will have a diagnosis of unexplained (idiopathic) infertility. This diagnosis means that, in spite of exhaustive fertility evaluation, there is no apparent cause of infertility.
Most of these patients have infertility factor(s) involving the eggs, sperm, and Fallopian tubes, but their testing has not yet uncovered this information. Infertility related to the egg quality factor represents most of the “unexplained” infertility since it is the most difficult one to diagnose.
In Vitro Fertilization is the most common treatment for patients with unexplained infertility.
Can endometriosis affect my fertility?
Endometriosis is a condition in which endometrial cells of the inner uterine lining can be found outside the uterus.
When there is a history of infertility, the female partner may have a laparoscopy. One-third of the time, endometriosis is found. The same incidence has been found in women undergoing laparoscopy for non-infertility reasons.
This finding, together with the lack of consistent scientific evidence that surgical or medical removal of endometriosis increases the probability of pregnancy, has led some clinicians to believe that endometriosis is merely a sign of another underlining cause of infertility.
A severe degree of endometriosis causes scarring around the Fallopian tubes and ovaries and can be an infertility factor.
What is PCOS?
t is estimated that perhaps 5% to 15% of all women are born with some degree of polycystic ovary syndrome (PCOS). Most of these women will never know since they will be able to conceive. These women have a mild degree of PCOS.
Women with more severe PCOS will, at least temporarily, lose the regularity of their menstruations (become anovulatory) and may need medical help to conceive. In its most severe forms, polycystic ovarian syndrome can make it quite difficult for a woman to ovulate and conceive, even with ovarian stimulation.
This lack of ovulation is accompanied by a hormonal imbalance which, in some women, involves abnormal insulin production and glucose metabolism.
How do you test egg quality?
We utilize a combination of transvaginal ultrasound examination of the ovaries and an assessment of reproductive hormones levels: Ovarian Reserve Assay (ORA) to estimate your “biological age.” The results of these tests will determine the most appropriate treatment for you.
The ultrasound examination of your ovaries determines the number of antral follicles (seen as small dark circles) within each ovary. The number of antral follicles is related to the quality of the eggs. Ideally, there should be approximately a total of 20 antral follicles in both ovaries.
ORA assesses the likelihood that normal-quality eggs can be produced. It consists of the measurement of Follicle Stimulating Hormone (FSH), estradiol (estrogen, E2), and Anti-Mullerian Hormone (AMH) blood levels.
What is premature ovarian failure, and can it be overcome?
“Premature ovarian failure refers to a loss of normal function of the ovaries before age 40. The ovaries can no longer produce normal quality eggs and female hormones estrogen and progesterone.
There is no known cure for premature ovarian failure, and most patients will need Donor Egg IVF treatment to conceive successfully.”
Does uterine receptivity affect pregnancy?
Uterine lining receptivity does not have a profound effect on the success of infertility treatments. The issue of uterine lining receptivity and its effect on pregnancy is one of the most frequently asked questions by our patients.
Studies that would implicate uterine receptivity as a major factor in infertility treatment success are lacking. On the other hand, there is evidence suggesting that the role of uterine lining receptivity as a decisive factor in human conception is limited.
What is Assisted Hatching, and what effect does it have on my embryos?
Assisted embryo hatching is a laboratory procedure that creates a “weak spot” in the eggshell of an embryo. For selected embryos, this increases the likelihood of the embryo being able to hatch out, implant, and result in a baby.
Assisted Hatching is a microsurgical procedure. Using a specially designed laser, a tiny hole is created in the eggshell. This procedure does not harm the embryo.
Is Carrier Genetic Screening recommended?
All future parents should consider genetic screening for over a hundred most common genetic diseases. Please let us know at the time of your initial appointment at Bay IVF if you wish to have your blood sample sent for genetic screening.
Carrier Genetic Screening is an important part of family planning. It can help you understand your risk of having a child with a genetic disease.
Typically carriers are healthy individuals, but when two parents are carriers of the same genetic disease, they can have a child affected with it. Unfortunately, most people do not know they are carriers until they have a child born with the disease.
Does acupuncture help with fertility?
Two recent studies found an increase in the conception rate among women undergoing acupuncture. A third study did not find a statistically significant improvement. It is possible to conclude from the available studies that acupuncture is safe for women undergoing advanced reproductive treatments.
What if I miss a Lupron injection?
This will probably not disturb your treatment. If you realize that you missed a dose before your next Lupron injection is due, take the missed dose when you remember and continue with your regular schedule. If you realize that you missed a dose when your next Lupron injection is due, skip the missed dose, do not double up, and continue with your regular schedule.
Can I take over-the-counter medications for a cold?
You can take Tylenol, Sudafed (regular), and Robitussin DM. Please contact our office if you need to take any other medications.
Can I take the flu vaccination during my treatment?
Yes, you can take the injectable form of the flu vaccine.
Can I eat sushi while trying to conceive?
Once pregnancy is achieved, we recommend that you do not eat uncooked fish (e.g., sushi) or undercooked shellfish, eggs, or meat.
I have a cat. May I change the litter box during my treatment?
To prevent becoming infected with toxoplasmosis, an infection that isn’t serious for you but can pose a danger to your developing baby. You should not change the litter of a cat litter box once you become pregnant. We also recommend that you use gloves and a mask when you garden. Be cautious around the sand in parks or playgrounds.
Can I dye my hair during my treatment?
Once your embryos have been transferred, we recommend that you do not dye your hair through the first trimester.
May I soak in a hot tub or use a sauna?
Once your ovarian stimulation starts, we recommend that you do not soak in a hot tub or use a sauna, due to the possible detrimental effect of high temperature.
Should I take time off work during IVF treatment?
You could, but it is not required that you do. Most patients will be able to continue their everyday lifestyles during their treatment.
Over the years, we have streamlined and simplified the process of In Vitro Fertilization to minimize interference with your lifestyle. As a result, an IVF treatment cycle can take as little as six to eight weeks and only requires a few brief visits to the Clinic.
You may want to take off the afternoon of your egg retrieval day, and that should be all the time off you should need.
Will my insurance cover the treatment?
Insurance plans vary widely. To determine if you have coverage for infertility treatments, we can call your insurance provider to confirm what benefits are available. You may also consider getting a loan for your fertility treatment.
Do I need an OB/GYN before starting IVF treatment?
Yes, you do. You may need to call on your OB/GYN for procedures related to your IVF treatment that are not part of your IVF treatment. An example might be an endometrial polyp removal if polyps are found during your prerequisites for IVF. You will also be referred to your obstetrician once your IVF treatment has been successful.
We look forward to meeting you at Bay IVF and, when your treatment is successful, celebrating your new pregnancy!
 +
+Years of Experience
 +
+Babies Born
 %
%Compassionate Care
Your Dream, Our Mission

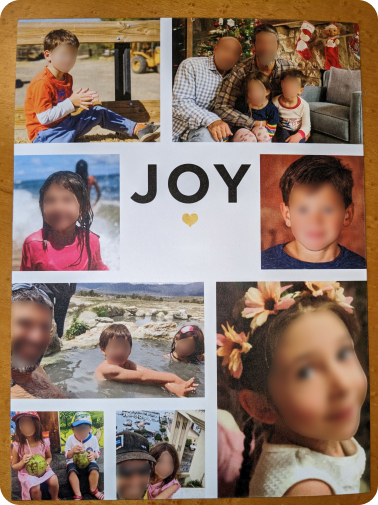
Hear from Our Patients’ Journey to Parenthood at Bay IVF!
I would highly recommend Bay IVF for those wanting to build their family and needing IVF support! Dr. Polansky and the whole Bay IVF team were so supportive and welcoming while also honest and realistic. Our girl is our dream come true!
Jennifer C.-F.This clinic has been amazing to work with. All the nurses and staff made sure I was always comfortable and were there to answer questions any time I needed. We are incredibly grateful to Dr. Polansky and the team for everything they did for us.
Harpreet K.Words could never express the gratitude my husband and I will always have for Bay IVF! We did our research and decided to check out Bay IVF. We scheduled a consultation and felt an instant connection… love at first sight!
Chelsea L.
Bay IVF Early Pregnancy Heartbeat

Meet Your Doctor

- Dr. Polansky received his medical diploma from Charles University in Prague, the Czech Republic, in 1978.
- After completing his OB/GYN residency at Jewish Hospital in Saint Louis, MO, he graduated from the Reproductive Endocrinology and Infertility (REI) fellowship at Stanford University in 1985.
- In the same year, he co-founded the Stanford IVF Clinic.
- Dr. Polansky obtained board certification in Obstetrics and Gynecology in 1986 and became REI subspecialty board certified in 1988.
- In 1987, he left Stanford University and established Nova IVF.
- In 2011, he founded Bay IVF, where he provides advanced fertility treatments with a holistic approach, utilizing state-of-the-art techniques.
- Dr. Polansky personally performs ultrasound examinations, egg retrievals, embryo transfers, and ovarian and endometrial stimulations for his patients.
- He is deeply committed to his patients and freely shares his cell phone number, ensuring accessibility and availability 24/7.
Frank Polansky, M.D.
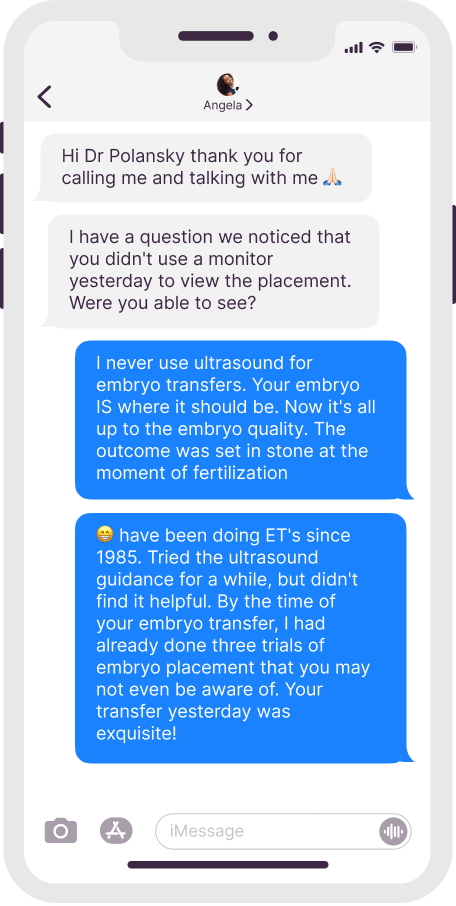
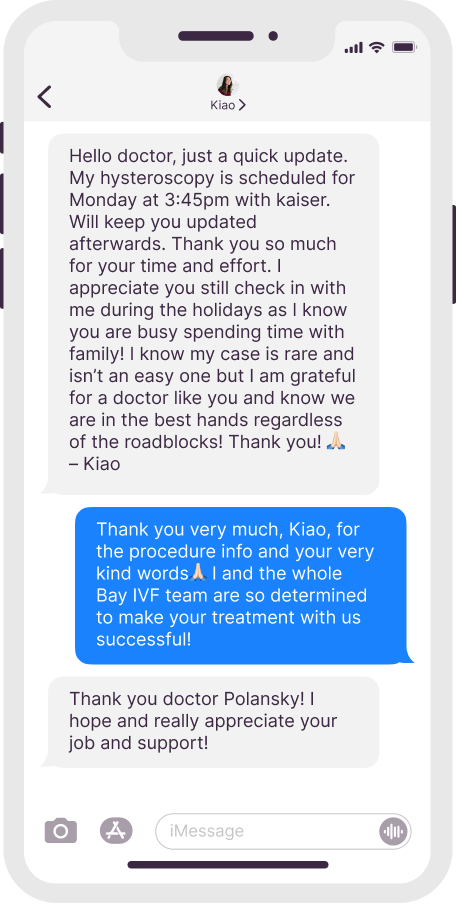
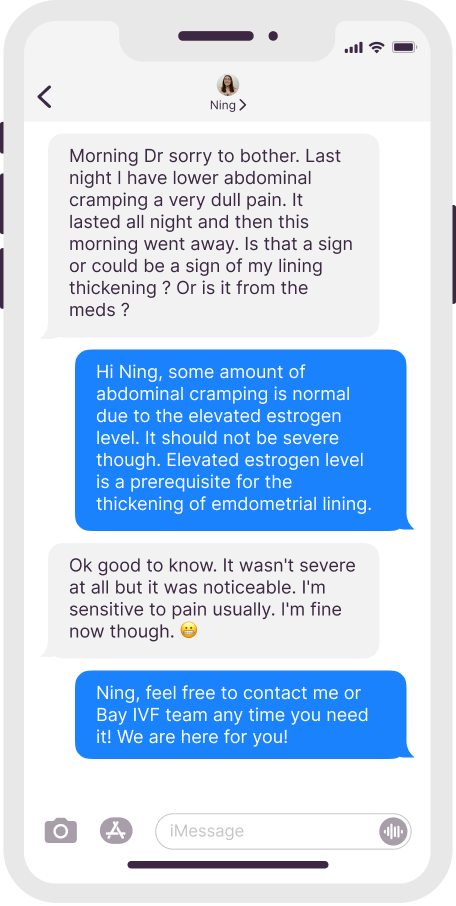
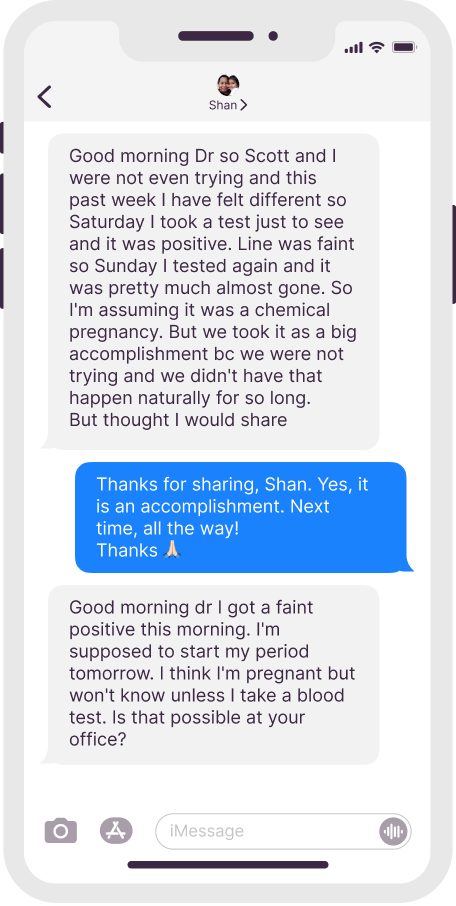
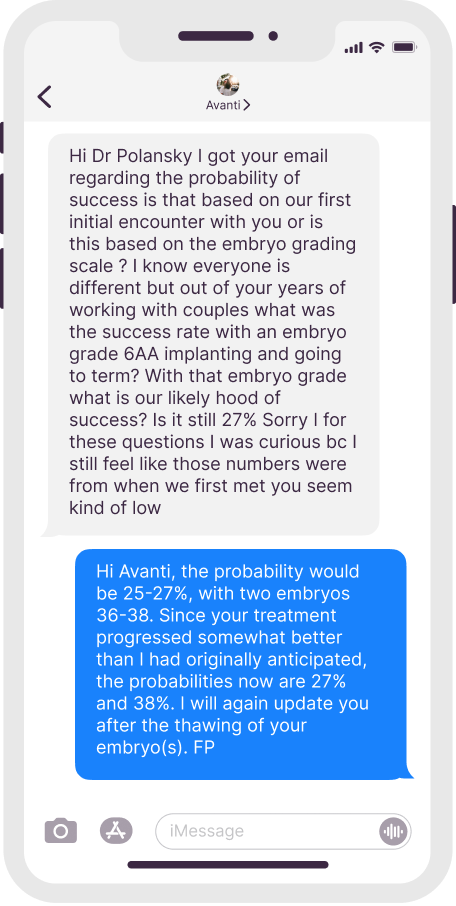
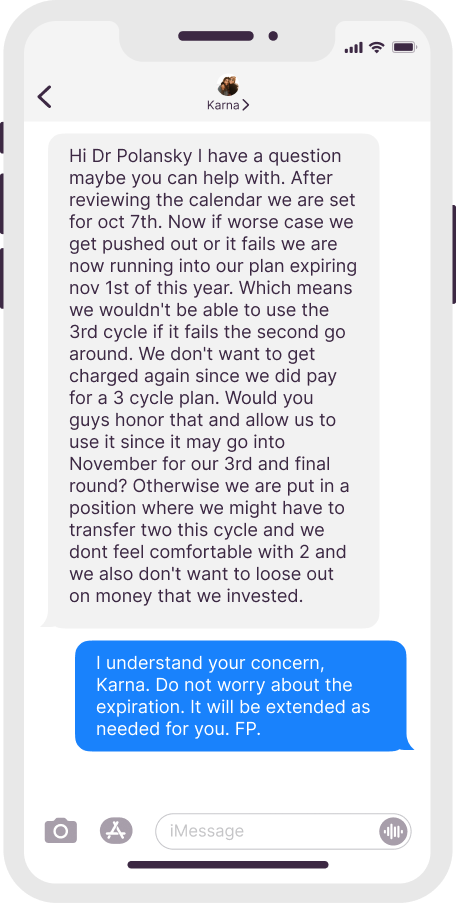
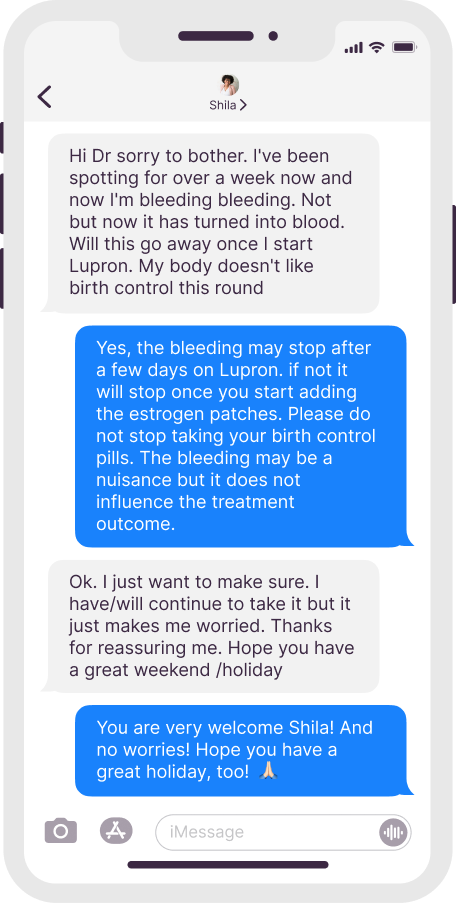
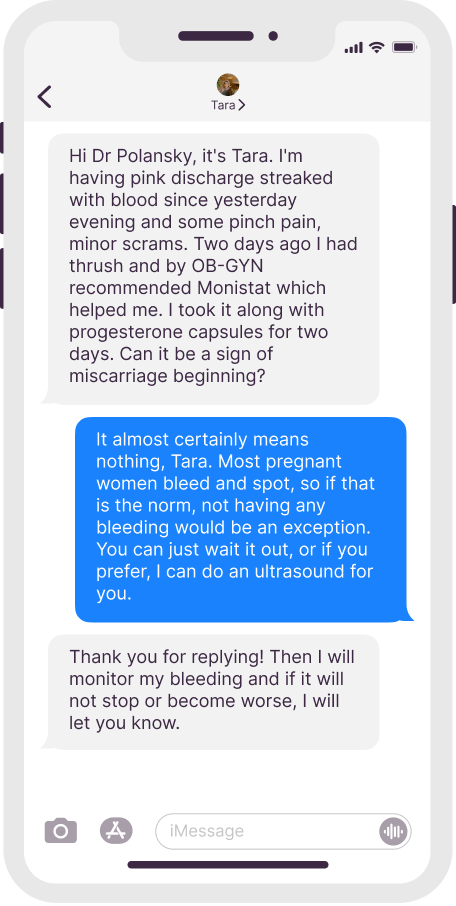
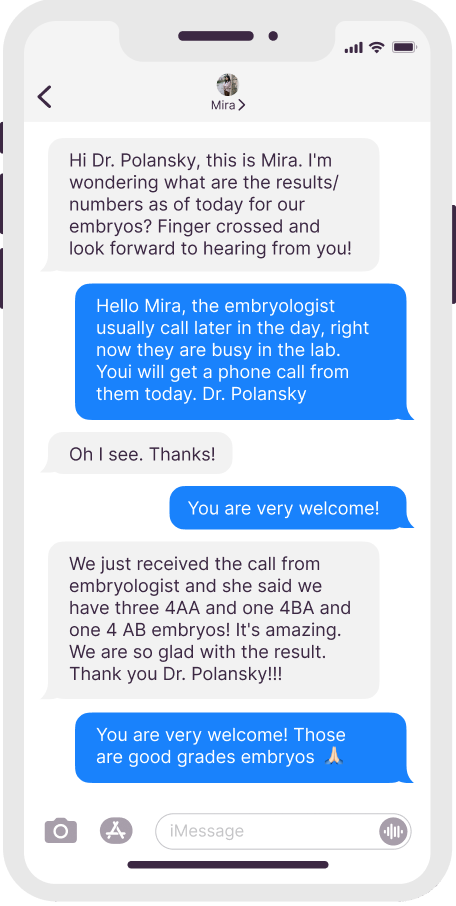
Dr. Polansky’s Communication With Patients
Real texts, anonymous patient names

Initial Appointment Questions
When you call to schedule your consultation, one of our Front Office Coordinators will ask you a short series of questions regarding your reproductive history.
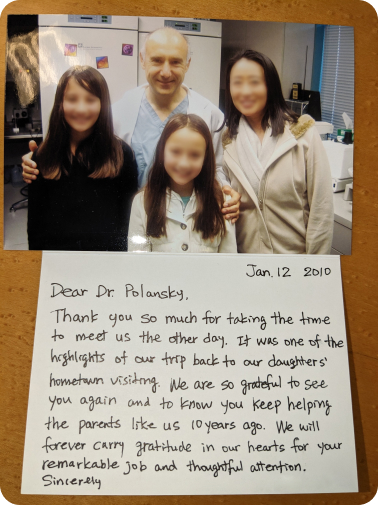
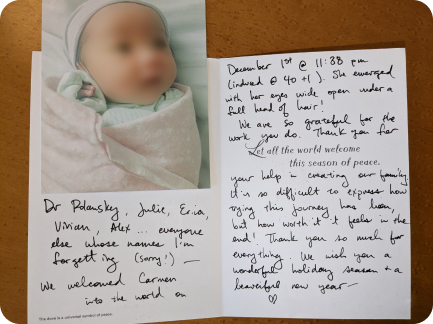
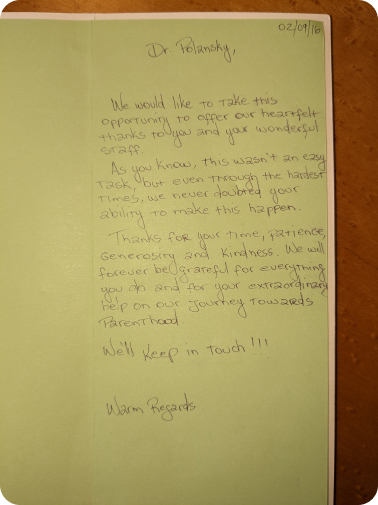
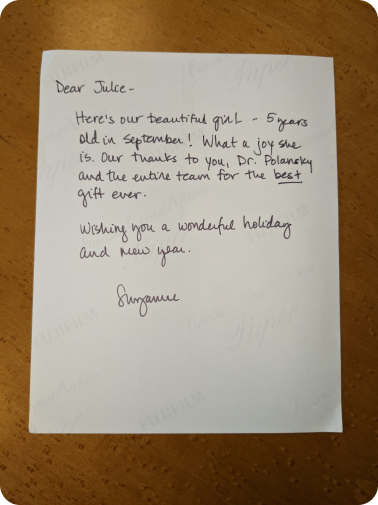
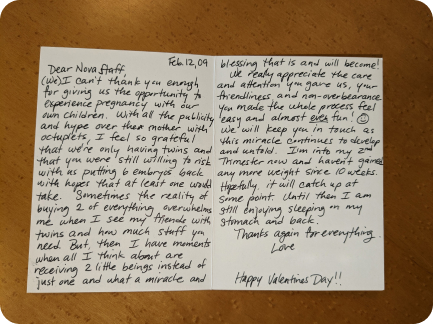
Patients’ Thank You Cards


Your Initial Visit at Bay IVF
Attending a new patient appointment at a fertility clinic can be stressful. Our primary objective is to ensure that your initial visit is friendly and relaxing. We encourage you to ask questions at every step of the process.
1 — When You Arrive
You will be welcomed by one of the clinic receptionists. One of our nurses will measure your height and weight and take your blood pressure

2 — Meet Your Doctor
Dr. Polansky will ask you a series of clarifying questions and then provide you with a summary of the factors contributing to your infertility

4 — Exam Room
One of the nurses will escort you to an examination room. Your examination will begin with listening to your lungs and heart

3 — Ask Your Questions
You will then have a discussion with him about the most suitable reproductive treatment(s) for you. During this time, you will have the opportunity to ask any questions you may have

5 — Ultrasound of the Ovaries
The next step is a pelvic ultrasound to examine the uterus and ovaries. This ultrasound will help determine the number of antral follicles present within the ovaries

6 — Financial Part
Following that, you will have a discussion with one of the financial advisors regarding the financial aspects of your treatment, including potential treatment financing options

8 — Support 24/7
If you have any questions after leaving the clinic, please feel free to reach out to us via phone call, text, or email. Open and discreet communication is an integral part of the care we provide at Bay IVF

7 — What About Time?
Your entire visit is expected to last approximately one hour

Schedule Your Initial Consultation With Dr. Polansky
Online (free) or In-Person
Call or Text Us: 650-322-0500
You can also complete the form below to request your initial consultation
Still Have Questions?
We understand that this is a significant decision, and it is important to us that you feel truly comfortable








