
In Vitro Fertilization
As an advanced IVF clinic, Bay IVF focuses on In Vitro Fertilization
Bringing a new baby into your life:
Will you join the 5 million patients worldwide who conceived with In Vitro Fertilization?
IVF is the most effective treatment to help patients achieve pregnancy from their own eggs and sperm.
In Vitro Fertilization
We use gentle, individualized ovarian stimulation protocols and strive for the highest egg quality rather than quantity.
This approach minimizes the number of clinic visits and decreases the likelihood of ovarian hyperstimulation without reducing the probability of a successful outcome.
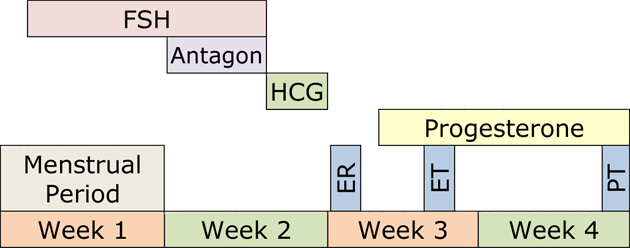
A cycle of IVF treatment can take as little as six weeks and only requires a few brief visits to the Clinic.
Most patients will be able to continue their everyday lifestyles during their treatment.

Indications for In Vitro Fertilization
You should consider IVF treatment if any of the following apply to you:

- History of tubal blockage or pelvic adhesions
- Male Factor Infertility
- Infertility associated with endometriosis
- Infertility associated with Polycystic Ovary Syndrome (PCOS)
- Unexplained infertility
- Long-standing infertility: no contraception for more than a year and a half
- Decreasing “ovarian reserve”
IVF may be the most appropriate treatment for women over the age of 37. - You did not become pregnant with intrauterine insemination (IUI) cycles.
- You did not become pregnant with ovarian stimulation cycles with oral or injectable medications.
Our goal is to make your conception experience pleasant, relaxed, and as natural as possible.
IVF Treatment Process
1 — Ovarian stimulation
Your treatment is always individualized to maximize the probability of a successful outcome. You will receive your personalized ovarian stimulation calendar.
2 — Egg retrieval procedure
The egg retrieval procedure is performed at our Clinic. The procedure typically takes only a few minutes, and we use conscious sedation for comfortable analgesia.
4 — Culture of embryos
Evidence of fertilization can be seen the next day, approximately 16 hours after insemination. The fertilized eggs are then transferred into a growth medium and continue to be cultured in our laboratory.
3 — Fertilization of eggs
On average, eight to fourteen eggs are retrieved during the egg retrieval procedure. Once identified, the eggs are combined with sperm and placed in petri dishes filled with culture medium.
5 — Embryo transfer
One or two embryos are carefully loaded into the tip of a thin embryo transfer catheter. The catheter is then guided through the cervix to the top of the endometrial cavity, where the embryo(s) are gently released.
6 —Embryo implantation
After the embryo transfer, the endometrial lining gently supports the embryo(s) within the top of the uterus. There are no restrictions on your physical activity.
Below is an example of an IVF treatment cycle. Your individualized protocol may take less or more time to complete.
In Vitro Fertilization Procedure

Ovarian stimulation
There are various forms of ovarian stimulation protocols, each with multiple modifications. Your treatment is always personalized to maximize the likelihood of success.
The optimal protocol for your IVF treatment is selected based on your reproductive history and your pre-treatment evaluation.
Ovarian stimulation takes approximately ten days. During this time, your progress is monitored by estradiol (estrogen, E2) and progesterone blood levels and ultrasound examinations.
Ovarian stimulation should result in the development of several eggs in each ovary. This ultrasound image shows a stimulated ovary. Each of the several follicles (dark circles) contains a microscopic egg.

Egg Retrieval Procedure
The egg retrieval procedure is performed at our Clinic. We provide comfortable, conscious sedation analgesia.
The egg retrieval is a quick and relatively painless procedure that takes about five minutes to complete. Here’s what happens during the procedure:
Administering Pain Medication
- Dr. Polansky administers pain medication and relaxation drugs through the IV line, inducing a state of twilight anesthesia.
- Most patients will fall asleep during the procedure, while some might remain awake and view the egg retrieval on an ultrasound screen.
Egg Retrieval Process
- Under ultrasound guidance, Dr. Polansky retrieves eggs from the ovaries using a thin needle passed through the top of the vagina.
- The needle aspirates the follicular fluid containing the eggs. The process is usually completed within minutes.
- Embryologists then examine the follicular fluid under a microscope to identify eggs.
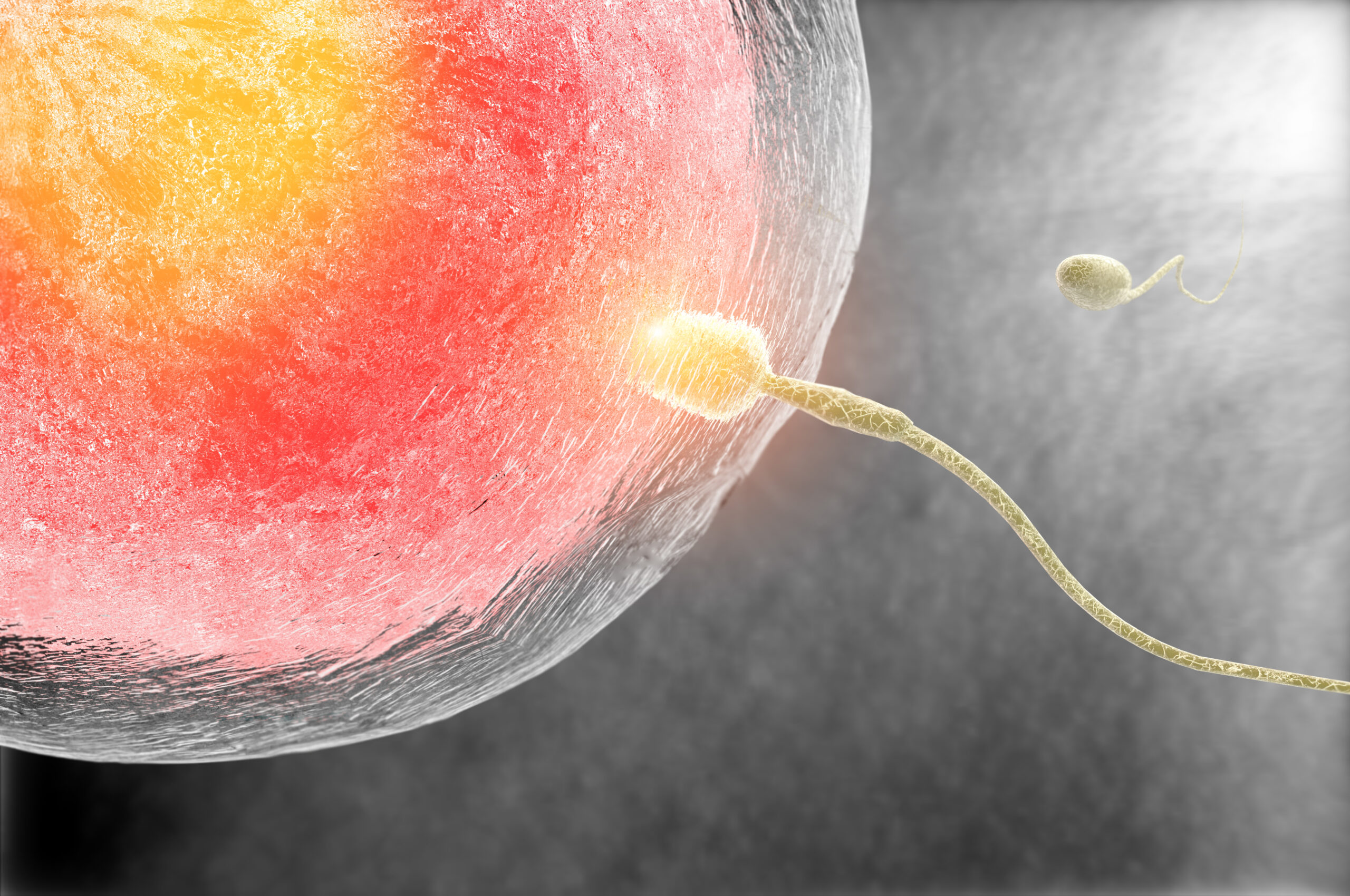
Fertilization of Eggs
On average, eight to fourteen eggs are retrieved during the egg retrieval procedure. Once identified, the eggs are placed in petri dishes filled with culture medium. The composition of the culture medium resembles the fluid secreted by the Fallopian tubes, facilitating the development of eggs and embryos (fertilized eggs) in our laboratory environment, simulating the conditions in the Fallopian tubes.
On the day of egg retrieval, the male partner provides a semen specimen through masturbation. The highest quality sperm are extracted from the semen and combined with the eggs three hours after retrieval. This in vitro fertilization process takes place over several hours in the evening following egg retrieval.
If the male partner has never caused pregnancy or if his test results indicate significant male infertility, Intracytoplasmic Sperm Injection (ICSI) is performed. In ICSI, a single sperm is directly injected into an egg, significantly increasing the probability of successful fertilization for selected patients.

Culture of Embryos
Fertilization is usually observed the day after insemination, approximately 16 hours later. A normally fertilized egg (zygote) will exhibit two pronuclei representing the genetic material from the egg and sperm. The fertilized eggs are transferred to a growth medium and continue to be cultured in our laboratory.
The following day, embryos should divide into 4 cells, and by the day after, they should reach 8 cells.
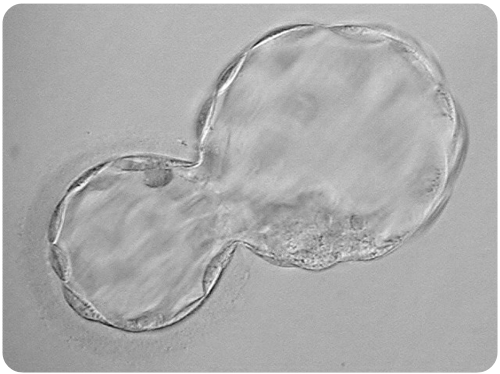
By the fifth to seventh day after the insemination, the embryos should develop into the blastocyst stage, consisting of 80 or more cells.
This picture shows an advanced stage of blastocyst development. Notice the central fluid-filled cavity. The cells within the blastocyst have already differentiated into the inner cell mass (at seven o’clock) that will give rise to the fetus and the trophectoderm cells that will form the future placenta.
At this stage, the embryos are still microscopic, invisible to the naked eye.

Embryo Transfer
The embryo transfer procedure typically occurs five days after egg retrieval, depending on the development of the embryos.
Prior to the transfer, our embryologists assess the embryos to determine their chances of successful implantation. This assessment helps you decide whether to transfer one or two embryos.
Just before the embryo transfer, the embryo(s) is/are placed into the tip of a thin embryo transfer catheter. The catheter is then passed through the cervical canal, reaching within 15 mm of the top of the uterine cavity, where the embryos are gently released.
The embryo transfer usually takes only a few seconds to complete, and no rest is required afterward.
In cases with more embryos than the intended number for transfer, these embryos can be frozen and stored in liquid nitrogen. The implantation success rate of frozen embryos is equal to that of “fresh”, unfrozen embryos.
Embryo implantation
After the embryo transfer, the endometrial lining gently holds the embryo(s) within the upper part of the uterus. There are no restrictions on your physical activity during this period.
This picture shows a healthy blastocyst in the process of “squeezing out” of its eggshell. Once fully hatched, it will stay in the uterus unattached for one to two days and then implant.
The lining of the uterus becomes receptive to the embryos through the action of estrogen and progesterone hormones produced by the ovaries. Ovarian progesterone production is supplemented with vaginal progesterone capsules.
A blood pregnancy test is scheduled two weeks after the embryo transfer. If the test is positive, an ultrasound examination is scheduled two weeks later to visualize the implantation site and check for a heartbeat within the embryo. Once a heartbeat is detected, there is a 95% probability that the pregnancy will result in a live birth.
Bay IVF Early Pregnancy Heartbeat

Prerequisites for In Vitro Fertilization
Only a few treatment prerequisites are needed before the start of your treatment. They assess the egg and sperm quality and ensure that embryos can be accurately placed in a healthy uterus.
Female partner’s age
The probability of a successful IVF treatment becomes exceedingly low by age 44. You must be 43 and 11 months or younger at the time your IVF treatment begins. Patients who are 44 and older should strongly consider Donor Egg IVF as the most effective treatment option to achieve a successful pregnancy.
Female partner’s weight
Your BMI must be no greater than 31 for an adequate ovarian response and safety during the egg retrieval procedure. If your BMI is higher, please follow the IVF Diet and Lifestyle (PDF) recommendations as closely as possible. By doing so, you can achieve weight loss at an optimal rate, which could significantly improve your chances of a successful pregnancy.
Pathogen testing
This testing is required by the State of California. You and your partner (if applicable) must be tested for Hepatitis B-Surface Antigen, Hepatitis C-Antibody, HIV I&II, HTLV I&II (male partner only), and RPR.
Ovarian Reserve Assay (ORA)
ORA assesses the likelihood of producing normal-quality eggs. It involves measuring Follicle Stimulating Hormone (FSH), estradiol (estrogen, E2), and Anti-Mullerian Hormone (AMH) blood levels.
These test results are used to optimize ovarian stimulation.
Antral Follicle Count
The number of antral follicles (small fluid-filled sacs within the ovaries seen on ultrasound) in unstimulated ovaries is related to the quality of the eggs. Ideally, there should be approximately 20 antral follicles in both ovaries combined.
Uterine measurement and saline ultrasound
It is important to determine the length of the uterus in order to ensure the correct placement of embryos.
A saline ultrasound is utilized to rule out the presence of intrauterine polyps or fibroids.
Semen evaluation
The male partner’s semen will be evaluated at Bay IVF to determine the best laboratory method for semen preparation for egg insemination.
Parents’ genetic testing (optional)
All prospective parents should consider genetic screening for hundreds of the most common genetic diseases. Please inform us during your initial appointment at Bay IVF if you would like to have your blood sample sent for genetic screening.
IVF diet and lifestyle
Environmental factors have a significant impact on reproductive health. Please review the IVF Diet and Lifestyle document (PDF) for a comprehensive list of environmental reproductive health recommendations and a source for dietary supplements.
Our sole goal is to ensure the success of your treatment!
FAQ — Find Answers to Your Queries
Here are some of the most commonly asked fertility-related questions. A more comprehensive FAQ selection is available on the FAQ page.
Should we transfer one or two embryos?
About half of our patients transfer two embryos at a time, while the other half choose to transfer only one embryo in each transfer. We will always provide guidance, but you will have the final say in whether to transfer one or two embryos.
What is gender selection treatment?
Gender selection is an extension of IVF treatment that utilizes the Pre-implantation Genetic Testing (PGT) procedure to identify the gender of each embryo. With this method, prospective parents can know the gender of each embryo with 100% accuracy prior to transfer into the uterus.
I am from the LGBTQ+ community. Can I have my treatment at Bay IVF?
Yes! We take pride in being one of the first fertility clinics in Northern California to offer In Vitro Fertilization services for lesbian partners. Our clinic is LGBTQ+ friendly and experienced in both lesbian IVF and Reciprocal IVF.
Is the egg retrieval procedure painful?
Your egg retrieval should be a very comfortable experience, as we use effective pain and relaxation medications. Most patients will sleep through the 5-10 minute egg retrieval procedure, though some may experience mild menstrual-like cramping.
What is the IVF cut-off age?
The probability of a successful IVF treatment becomes exceedingly low by age 44. You must be 43 and 11 months or younger at the time your IVF treatment begins. Patients who are 44 and older should strongly consider Donor Egg IVF as the most effective treatment option to achieve a successful pregnancy.
I am over 44, but my ovarian reserve is very good. Can I do IVF treatment?
We have occasionally provided IVF treatment to women over the age of 44 when their antral follicle count and AMH results suggest that their eggs are biologically younger than their chronological age.
What are the BMI requirements?
Your BMI must be no greater than 31 for an adequate ovarian response and safety during the egg retrieval procedure. If your BMI is higher, please follow the IVF Diet and Lifestyle (PDF) recommendations as closely as possible. Doing so can help you achieve weight loss at an optimal rate, which could significantly improve your chances of a successful pregnancy.
Do you offer payment plans?
Our IVF Duo and IVF Trio Financial Plans can provide substantial savings compared with single-cycle IVF fees. Two- and three-cycle financial plans for Egg Freezing are also available.
Bay IVF has partnered with Future Family to offer accessible, personal, and affordable fertility care financing. Their mission is to make fertility care more accessible and affordable. Future Family loans are an alternative to high-interest credit cards and dipping into your savings. They offer 0% APR financing for those who are eligible, as well as low monthly payment plans. Prequalifying is risk-free, easy, and will not affect your credit score.
Meet Your Doctor

- Dr. Polansky received his medical diploma from Charles University in Prague, the Czech Republic, in 1978.
- After completing his OB/GYN residency at Jewish Hospital in Saint Louis, MO, he graduated from the Reproductive Endocrinology and Infertility (REI) fellowship at Stanford University in 1985.
- In the same year, he co-founded the Stanford IVF Clinic.
- Dr. Polansky obtained board certification in Obstetrics and Gynecology in 1986 and became REI subspecialty board certified in 1988.
- In 1987, he left Stanford University and established Nova IVF.
- In 2011, he founded Bay IVF, where he provides advanced fertility treatments with a holistic approach, utilizing state-of-the-art techniques.
- Dr. Polansky personally performs ultrasound examinations, egg retrievals, embryo transfers, and ovarian and endometrial stimulations for his patients.
- He is deeply committed to his patients and is always ready to lend a helping hand.
Frank Polansky, M.D.

Initial Appointment Questions
When you call to schedule your consultation, one of our Front Office Coordinators will ask you a short series of questions regarding your reproductive history.
Your Initial Visit at Bay IVF
Attending a new patient appointment at a fertility clinic can be stressful. Our primary objective is to ensure that your initial visit is friendly and relaxing. We encourage you to ask questions at every step of the process.
1 — When You Arrive
You will be welcomed by one of the clinic’s receptionists. One of our nurses will measure your height and weight and take your blood pressure

2 — Meet Your Doctor
Dr. Polansky will ask you a series of clarifying questions and then provide you with a summary of the factors contributing to your infertility

4 — Exam Room
One of the nurses will escort you to an examination room. Your examination will begin with listening to your lungs and heart

3 — Ask Your Questions
You will then have a discussion with him about the most suitable reproductive treatment(s) for you. During this time, you will have the opportunity to ask any questions you may have

5 — Ultrasound of the Ovaries
The next step is a pelvic ultrasound to examine the uterus and ovaries. This ultrasound will help determine the number of antral follicles present within the ovaries

6 — Financial Part
Following that, you will have a discussion with one of the financial advisors regarding the financial aspects of your treatment, including potential treatment financing options

8 — Support 24/7
If you have any questions after leaving the clinic, please feel free to reach out to us via phone call, text, or email. Open and discreet communication is an integral part of the care we provide at Bay IVF

7 — What About Time?
Your entire visit is expected to last approximately one hour
Schedule Your Initial Consultation With Dr. Polansky
Online (No Cost) or In-Person
Call or Text Us: 650-322-0500
You can also complete the form below to request your initial consultation
We look forward to meeting you at Bay IVF and, when your treatment is successful, celebrating your new pregnancy!








