
What Is Gestational Surrogacy
In Gestational Surrogacy, the intended mother or an egg donor provides the eggs, and the intended father provides the sperm. IVF is done to create embryos, which are subsequently transferred into the surrogate’s uterus.

There are numerous reasons why individuals and couples turn to Gestational Surrogacy. Medical conditions like uterine abnormalities or chronic illnesses can prevent some women from carrying a pregnancy. Women who had a hysterectomy can also find parenthood through this path.
There are two kinds of surrogacy pregnancies. In Traditional Surrogacy, the surrogate is artificially inseminated with semen from the intended father (or a sperm donor). The surrogate provides both the egg and carries the pregnancy for the intended parents. The baby is genetically linked to the intended father and the surrogate but not to the intended mother. The surrogate is both the gestational carrier and the biological mother of the child.
Gestational Surrogacy, on the other hand, separates the genetic material of the surrogate from the intended parents. In this method, the surrogate carries an embryo created using the eggs and sperm of the intended parents or donors. The embryo is implanted into the surrogate’s uterus through In Vitro Fertilization (IVF), allowing the surrogate to carry and nurture the child without a genetic connection.
It is important to understand the key differences between Gestational and Traditional Surrogacy:
- Genetic Connection
- Traditional Surrogacy: The surrogate is genetically related to the child.
- Gestational Surrogacy: The surrogate is not genetically related to the child.
- Legal Implications
- Traditional Surrogacy: Legal complexities may arise as the surrogate is genetically related to the child, potentially leading to custody issues.
- Gestational Surrogacy: The legal process is often smoother, as the surrogate has no genetic ties to the child.
- Emotional Dynamics
- Traditional Surrogacy: Emotional complexities can arise due to the genetic connection between the surrogate and the child.
- Gestational Surrogacy: Emotional boundaries are often clearer as there is no genetic link, promoting a more straightforward relationship.
- Medical Procedures
- Traditional Surrogacy: Involves artificial insemination.
- Gestational Surrogacy: Requires in vitro fertilization (IVF) to create an embryo for implantation.
Choosing between Traditional and Gestational Surrogacy is a deeply personal decision involving the journey’s emotional, legal, and medical aspects. Understanding the differences between these two approaches is crucial for individuals or couples exploring surrogacy as a path to parenthood.
Finding a surrogate is the first step in initiating the Gestational Surrogacy treatment. You may decide to use one of the many surrogacy agencies nationwide. These agencies have pre-selected surrogates for you to choose from.
Pursuing Gestational Surrogacy is a complex journey with emotional, financial, and legal hurdles. Intended parents must navigate a maze of surrogacy agencies, legal contracts, and medical procedures. The surrogate undergoes rigorous screening and medical evaluations, ensuring her physical and mental well-being throughout the process. The legal contracts detail the rights and responsibilities of all parties involved, providing legal clarity and emotional security.
Gestational Surrogacy is a two-stage treatment. The first phase consists of the development and cryopreservation of embryos:
- Ovarian Stimulation (Intended Mother or Egg Donor)
- Egg Retrieval Procedure
- Fertilization of eggs
- Culture of embryos
- Cryopreservation of embryos
- Embryo storage
The second stage consists of the Frozen Embryo Transfer cycle.
Ovarian Stimulation: There are several different forms of ovarian stimulation protocols, each with many modifications. The treatment is always individualized to maximize the probability of a successful outcome.
An optimal protocol is selected based on one’s reproductive history and pre-treatment evaluation. Below is an example of a Gestational Surrogacy treatment protocol. Your individualized protocol may take less or more time to complete.
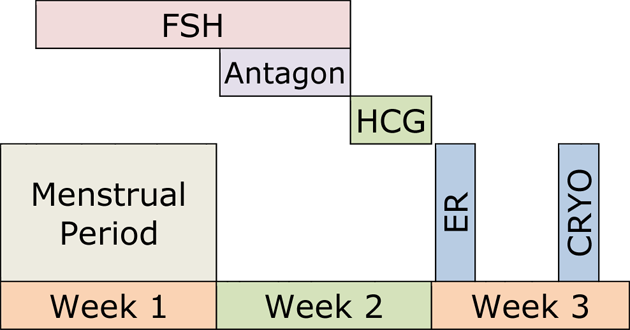
Follicle-stimulating hormone (FSH) or a combination of FSH/luteinizing hormone (LH) hormones will stimulate the production of multiple eggs in the ovaries. They are given subcutaneously once a day or every other day with tiny needles for approximately ten days.
During this time, progress is monitored by measuring estradiol (estrogen, E2) and progesterone blood levels, as well as through ultrasound examinations.
Ovarian stimulation should result in the development of several eggs in each ovary. The ultrasound image below shows a stimulated ovary. Each of the several follicles (dark circles) contains a microscopic egg.

Egg Retrieval Procedure: The egg retrieval procedure is performed at our Center. The procedure only takes a few minutes, and we use very comfortable conscious sedation for analgesia.
Since 1985, we have done many thousands of egg retrievals and are very experienced in retrieving eggs from the ovaries.
Under ultrasound guidance, the tip of a thin needle is passed through the top of the vagina into the cul-de-sac (space behind the uterus). The ovaries are located near the bottom of the cul-de-sac, allowing the tip of the aspirating needle to enter the ovarian follicles and aspirate the follicular fluid from them. The fluid is examined under a microscope to identify the eggs.
Fertilization of Eggs: On average, twelve to sixteen eggs are aspirated during the egg retrieval procedure. The eggs are identified under the microscope and placed in petri dishes filled with culture medium. The composition of the medium resembles the fluid secreted by the Fallopian tubes. This allows the eggs and embryos (fertilized eggs) to develop in our laboratory environment at the same rate as inside the Fallopian tubes.
The intended father’s sperm was already collected and cryopreserved. On the day of egg retrieval, a portion of the frozen semen is thawed, and the highest quality sperm are extracted from the semen and combined with the eggs three hours after the egg retrieval. This process of in vitro fertilization takes place over several hours during the evening after egg retrieval.
If the intended father has never caused pregnancy, or if the test results indicate a possibility of significant male infertility, Intracytoplasmic Sperm Injection (ICSI) is performed. In ICSI, a single sperm is inserted into an egg. This can substantially increase the probability of successful fertilization for selected patients.
Culture of Embryos: Evidence of fertilization can be seen the next day, 16 hours after insemination. The fertilized eggs are transferred into a growth medium and continue to be cultured in our laboratory.
A normally fertilized egg (zygote) will show two pronuclei representing the genetic material from the egg and sperm.
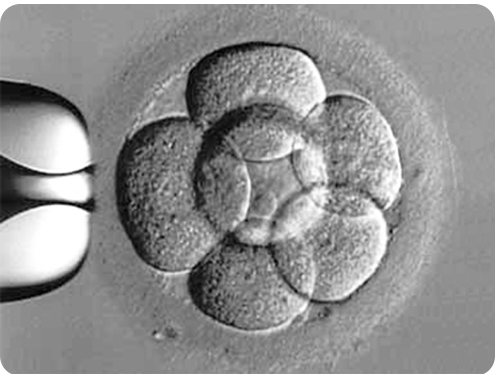
The following day, embryos should divide into 4 cells and, the day after, into 8 cells.
This picture shows a morphologically exquisite, day three, 8-cell embryo. Human embryos are still microscopic and invisible to the naked eye at this stage.
Embryos should reach the blastocyst stage (80 or more cells) by the fifth to seventh day after insemination.
This picture shows an advanced stage of blastocyst development. Notice the central fluid-filled cavity. The cells within the blastocyst have already differentiated into the inner cell mass (at seven o’clock) that will give rise to the fetus and the trophectoderm cells that will form the future placenta.

Cryopreservation of Embryos: Embryos that develop normally are cryopreserved (vitrified). Preparation for the freezing process involves removing water from within the embryos and replacing it with a cryoprotective substance to prevent ice crystal formation during vitrification and subsequent thawing. The embryos are then flash-cooled to −196 °C (−321 °F). Such rapid freezing (vitrification) prevents damaging water crystal formation.
Embryo Storage: Following cryopreservation, the embryos are transferred to a liquid nitrogen storage chamber in our Center. Theoretically, there is no limit on the length of storage, but conceiving past the age of 40 may result in a high-risk pregnancy.
Once you decide to use your cryopreserved embryos, one or two embryos will be thawed and transferred into the surrogate’s uterus. A large majority of the embryos will survive the vitrification and thawing process. The implantation rate of the thawed embryos should be the same as the “fresh” embryo implantation rate.
Despite the complexities and challenges, the conclusion of the gestational surrogacy journey often culminates in a moment of sheer joy and fulfillment—the birth of a child.
Meet Your Doctor

- Dr. Polansky received his medical diploma from Charles University in Prague, the Czech Republic, in 1978.
- After completing his OB/GYN residency at Jewish Hospital in Saint Louis, MO, he graduated from the Reproductive Endocrinology and Infertility (REI) fellowship at Stanford University in 1985.
- In the same year, he co-founded the Stanford IVF Clinic.
- Dr. Polansky obtained board certification in Obstetrics and Gynecology in 1986 and became REI subspecialty board certified in 1988.
- In 1987, he left Stanford University and established Nova IVF.
- In 2011, he founded Bay IVF, where he provides advanced fertility treatments with a holistic approach, utilizing state-of-the-art techniques.
- Dr. Polansky personally performs ultrasound examinations, egg retrievals, embryo transfers, and ovarian and endometrial stimulations for his patients.
- He is deeply committed to his patients and freely shares his cell phone number, ensuring accessibility and availability 24/7.
Frank Polansky, M.D.

Initial Appointment Questions
When you call to schedule your consultation, one of our Front Office Coordinators will ask you a short series of questions regarding your reproductive history.
Your Initial Visit at Bay IVF
Attending a new patient appointment at a fertility clinic can be stressful. Our primary objective is to ensure that your initial visit is friendly and relaxing. We encourage you to ask questions at every step of the process.
1 — When You Arrive
You will be welcomed by one of the clinic receptionists. One of our nurses will measure your height and weight and take your blood pressure

2 — Meet Your Doctor
Dr. Polansky will ask you a series of clarifying questions and then provide you with a summary of the factors contributing to your infertility

4 — Exam Room
One of the nurses will escort you to an examination room. Your examination will begin with listening to your lungs and heart

3 — Ask Your Questions
You will then have a discussion with him about the most suitable reproductive treatment(s) for you. During this time, you will have the opportunity to ask any questions you may have

5 — Ultrasound of the Ovaries
The next step is a pelvic ultrasound to examine the uterus and ovaries. This ultrasound will help determine the number of antral follicles present within the ovaries

6 — Financial Part
Following that, you will have a discussion with one of the financial advisors regarding the financial aspects of your treatment, including potential treatment financing options

8 — Support 24/7
If you have any questions after leaving the clinic, please feel free to reach out to us via phone call, text, or email. Open and discreet communication is an integral part of the care we provide at Bay IVF

7 — What About Time?
Your entire visit is expected to last approximately one hour
Schedule Your Initial Consultation With Dr. Polansky
Online (no cost) or In-Person
Call or Text Us: Call or text us at 📞 650 322 0500
You can also complete the form below to request your initial consultation.
We look forward to meeting you at Bay IVF and, when your treatment is successful, celebrating your new pregnancy!








